Joint pain can turn simple tasks into daily challenges, especially when it’s caused by osteoarthritis. As the most common form of arthritis, osteoarthritis affects millions, especially those in middle age and older. It’s a chronic condition that wears down the cartilage in your joints, leading to pain, stiffness, and reduced mobility—most often in your knees, hips, hands, and spine.
You might notice that pain limits your movement or makes it tough to enjoy activities you love. But managing osteoarthritis isn’t just about living with discomfort. With the right strategies—like exercise, weight control, and therapy—you can take charge of your symptoms and improve your quality of life. Understanding how osteoarthritis works and what you can do about it is the first step toward feeling better every day.
What Is Osteoarthritis?
Osteoarthritis is a chronic joint disease that breaks down cartilage and affects millions. Cartilage cushions the ends of your bones, so when it deteriorates, bones rub together and you feel pain, stiffness, and reduced flexibility. Most often, osteoarthritis targets your knees, hips, hands, and spine.
Symptoms of osteoarthritis include joint pain after movement, morning stiffness that lasts under 30 minutes, and swelling or tenderness in the affected joints. Over time, you might notice a decrease in your range of motion or even a grating sensation as the joint moves.
Osteoarthritis differs from osteoporosis since it affects joint cartilage and not bone density. While it progresses slowly, osteoarthritis causes daily discomfort for many and can limit your activities if it's left unmanaged.
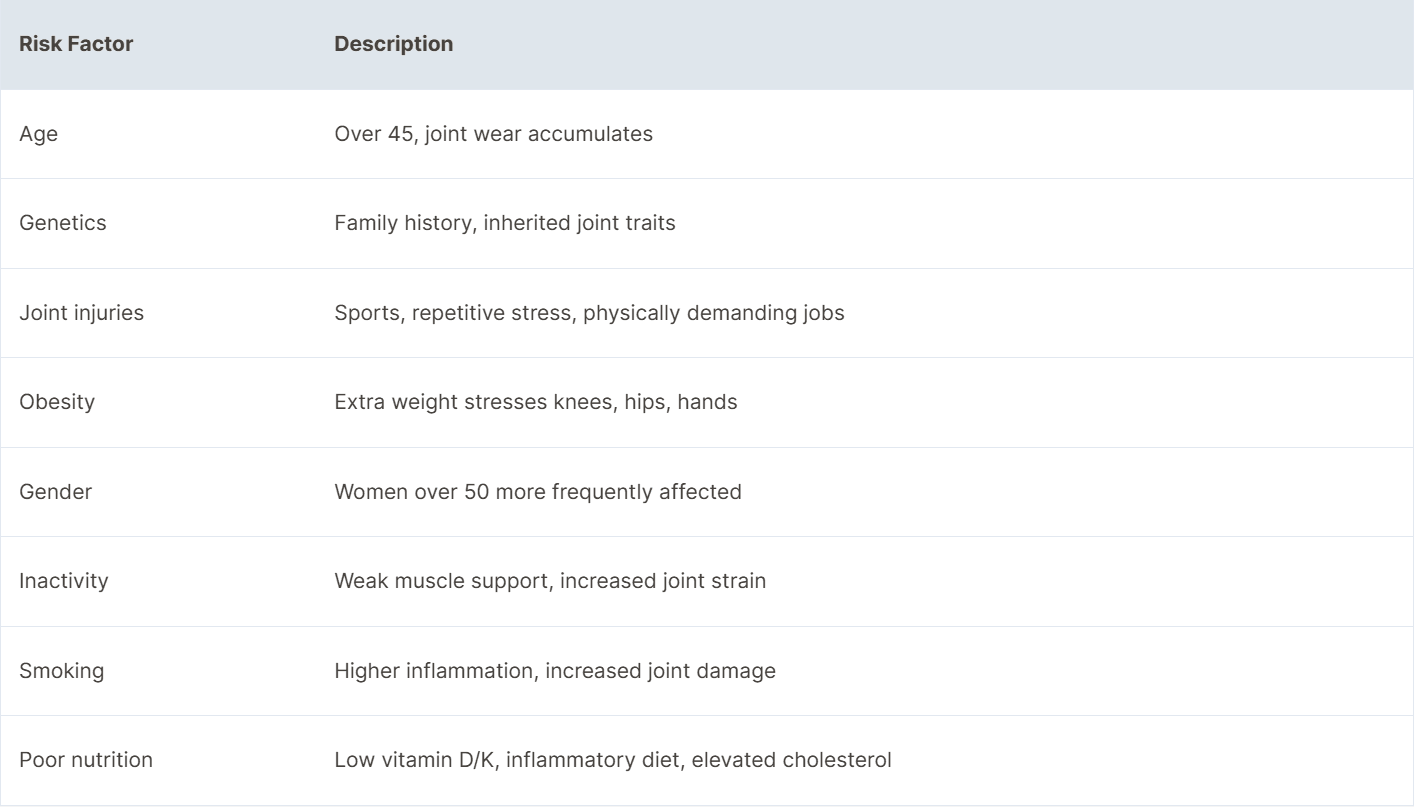
Causes and Risk Factors
Aging increases your risk of developing osteoarthritis, with most cases found in adults over 45 due to the cumulative wear and tear on joint cartilage. Genetics influence your likelihood as well—family history and inherited joint traits raise susceptibility. Joint injuries elevate risk, whether from sports accidents or repetitive stress in physically demanding jobs like flooring installation, with knees and hips affected most often.
Obesity contributes to osteoarthritis by adding pressure to weight-bearing joints such as knees and hips and links directly to hand osteoarthritis through inflammatory processes. Gender plays a role; data show women over 50 are more likely to develop osteoarthritis than men of the same age. Inactivity and weak supporting muscles make your joints more vulnerable, especially when combined with poor nutrition or deficiencies in vitamin D and K.
Smoking is associated with increased inflammation and joint damage. Elevated cholesterol levels and inflammatory diets may also play roles in osteoarthritis development. Certain chronic repetitive movements or heavy lifting over time can accelerate joint breakdown, particularly if any underlying joint abnormality exists.
Recognizing Symptoms and Diagnosis
Osteoarthritis often starts with subtle joint changes before pain or stiffness becomes obvious. Identifying early symptoms and seeking an accurate diagnosis helps you manage and slow disease progression.
Common Signs to Watch For
Common osteoarthritis symptoms affect daily activities and mobility. Joint pain during or after movement occurs most frequently in knees, hips, hands, and spine. Stiffness usually follows periods of inactivity, often lasting less than 30 minutes after waking. Joint swelling and tenderness develop as cartilage wears down. You might notice a reduced range of motion, muscle weakness around the joint, or a grating sensation—called crepitus—when moving. In some instances, joints feel unstable or appear enlarged. Symptoms fluctuate and often worsen with overuse, weather changes, or advancing age.
How Osteoarthritis Is Diagnosed
Healthcare professionals diagnose osteoarthritis with a combination of history, physical exam, and imaging. Your provider starts by reviewing your symptoms, medical background, and any joint injuries. Physical exams include checking for tenderness, swelling, joint alignment, and movement restrictions. Imaging tests—such as X-rays—detect cartilage loss, joint space narrowing, or bone spurs characteristic of osteoarthritis. Advanced cases may use MRI for detailed soft tissue assessment if X-rays are inconclusive. Occasionally, laboratory tests such as bloodwork or joint fluid analysis rule out other forms of arthritis, including rheumatoid arthritis or infection. Accurate diagnosis ensures the most effective personalized management plan.
Approaches to Managing Joint Pain
Managing joint pain from osteoarthritis takes a multi-faceted, individualized approach. Combining lifestyle changes, targeted therapies, and medical interventions helps address symptoms and maintain mobility.
Lifestyle Modifications
Lifestyle modifications lessen osteoarthritis joint pain and improve joint function. Weight loss reduces pressure on knees and hips if you're overweight. Regular low-impact exercise—examples include swimming, walking, and cycling—builds muscle strength around joints, enhances balance, and preserves flexibility. Activity consistency delivers better, longer-lasting benefits. Using assistive devices or joint protection techniques—wearing cushioned insoles, using canes, avoiding repetitive movements—limits excessive joint strain. Heat or cold therapy manages local pain or swelling, with heating pads and cold packs as common tools. Keeping a symptom journal enables tracking of triggers and effectiveness of management strategies.
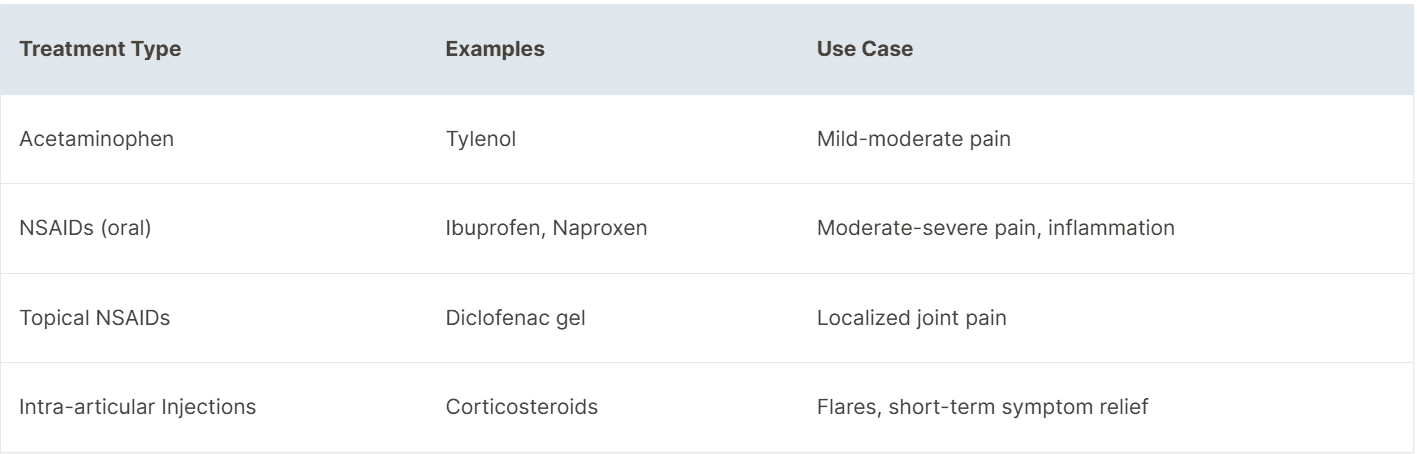
Medical Treatments and Therapies
Medical treatments and therapies offer options for controlling osteoarthritis joint pain when lifestyle changes aren’t enough. OTC pain relievers like acetaminophen or NSAIDs handle mild to moderate pain. Topical NSAIDs—gels or creams—target pain in a specific joint and have a lower risk of systemic side effects. Severe pain sometimes requires short-term corticosteroid joint injections. Physical therapy creates tailored exercise plans to gain strength, increase range of motion, and reduce discomfort. Occupational therapy teaches techniques for easier movement and joint protection in daily tasks. Medications focus on pain control and symptom relief; disease-modifying treatments remain under clinical investigation.
Table: Pharmacological Approaches
Surgical Options
Surgical options address severe osteoarthritis pain and loss of function when other approaches fail. Joint replacement surgery, such as knee or hip replacement, restores mobility and reduces pain in advanced cases. Specialist evaluation determines suitability, considering pain severity, disability, and failure of non-surgical treatments. Arthroscopy isn’t recommended for most with osteoarthritis due to limited benefit. Rehabilitation after joint surgery involves physical therapy to optimize recovery and function.
Self-Care and Preventive Strategies
Self-care and preventive strategies reduce osteoarthritis joint pain and slow symptom progression.
- Consistent Physical Activity
Regular low-impact exercise, for example swimming, cycling, or tai chi, strengthens muscles that support joints and improves flexibility. Movement reduces stiffness and pain, especially in weight-bearing joints like knees and hips.
- Weight Management
Maintaining a healthy weight lowers the load on joints and decreases inflammation. Every pound lost relieves up to four pounds of pressure on knee joints, contributing to lower pain scores among overweight individuals.
- Joint Protection
Using supportive footwear, braces, or walking aids minimizes stress on joints and prevents further injury during daily activities. Adaptive devices, such as jar openers for hand osteoarthritis, protect joint structure.
- Heat and Cold Therapy
Applying warm packs eases muscle tension and joint stiffness, while cold packs reduce inflammation and swelling after activity.
- Symptom and Activity Tracking
Keeping a symptom journal or step counter helps monitor flare-ups and identify effective strategies. Recording daily pain scores, activity levels, and triggers enables more tailored care adjustments.
- Support and Stress Management
Joining support groups connects you with others managing osteoarthritis, improving motivation and sharing proven coping methods. Practicing relaxation—like deep breathing or meditation—lowers stress, which can otherwise worsen joint pain.
- Education and Professional Guidance
Learning about osteoarthritis from trusted sources empowers informed decisions. Working with physical or occupational therapists provides guidance on safe exercises and techniques to protect your joints, maximizing self-management results.
The most effective self-care strategies depend on regular practice and ongoing evaluation, tailored to how osteoarthritis symptoms change over time.
Living Well With Osteoarthritis
You create better daily experiences with osteoarthritis by combining movement, self-care, and support. Daily habits play a central role in managing joint pain and maintaining independence.
- Stay Active
Regular low-impact activity, such as swimming, cycling, or walking, builds strength in muscles around affected joints. These exercises improve flexibility and reduce pain, as shown in controlled studies from Mayo Clinic and Arthritis Foundation.
- Maintain Healthy Weight
Reducing excess weight decreases pressure on knees and hips, leading to less pain and better mobility. Data indicate that weight loss of 5%–10% from body weight can result in measurable reductions in joint discomfort among people with osteoarthritis.
- Practice Joint Protection
Using assistive tools, for example canes or jar openers, prevents unnecessary strain on joints. Protective footwear and cushioned insoles help absorb impact during movement. Simple modifications like these extend joint function.
- Use Heat and Cold Therapy
Applying heat packs addresses stiffness and relaxes muscles before activities. Cold packs reduce swelling and numb sharp pain after use. This technique can be performed several times per day for targeted relief.
- Focus on Stress Management
Practicing relaxation methods, such as meditation or deep breathing, reduces emotional stress, which links to the severity of osteoarthritis pain. Support groups and online communities connect you with peers for encouragement and practical insight.
- Optimize Sleep Quality
Managing pain improves sleep quality, which in turn helps reduce fatigue and pain sensitivity. Sleep routines, for instance limiting screen time and sticking to scheduled hours, support better rest.
- Monitor Your Symptoms
Keeping a daily symptom and activity journal highlights patterns and identifies triggers of discomfort. This record assists healthcare professionals in adjusting your care for optimal results.
- Consult Professionals
Partnering with physical or occupational therapists yields personalized exercises and guidance. You can partner with us at Pristines to get recommendations for activity modifications based on the latest research and clinical guidelines.
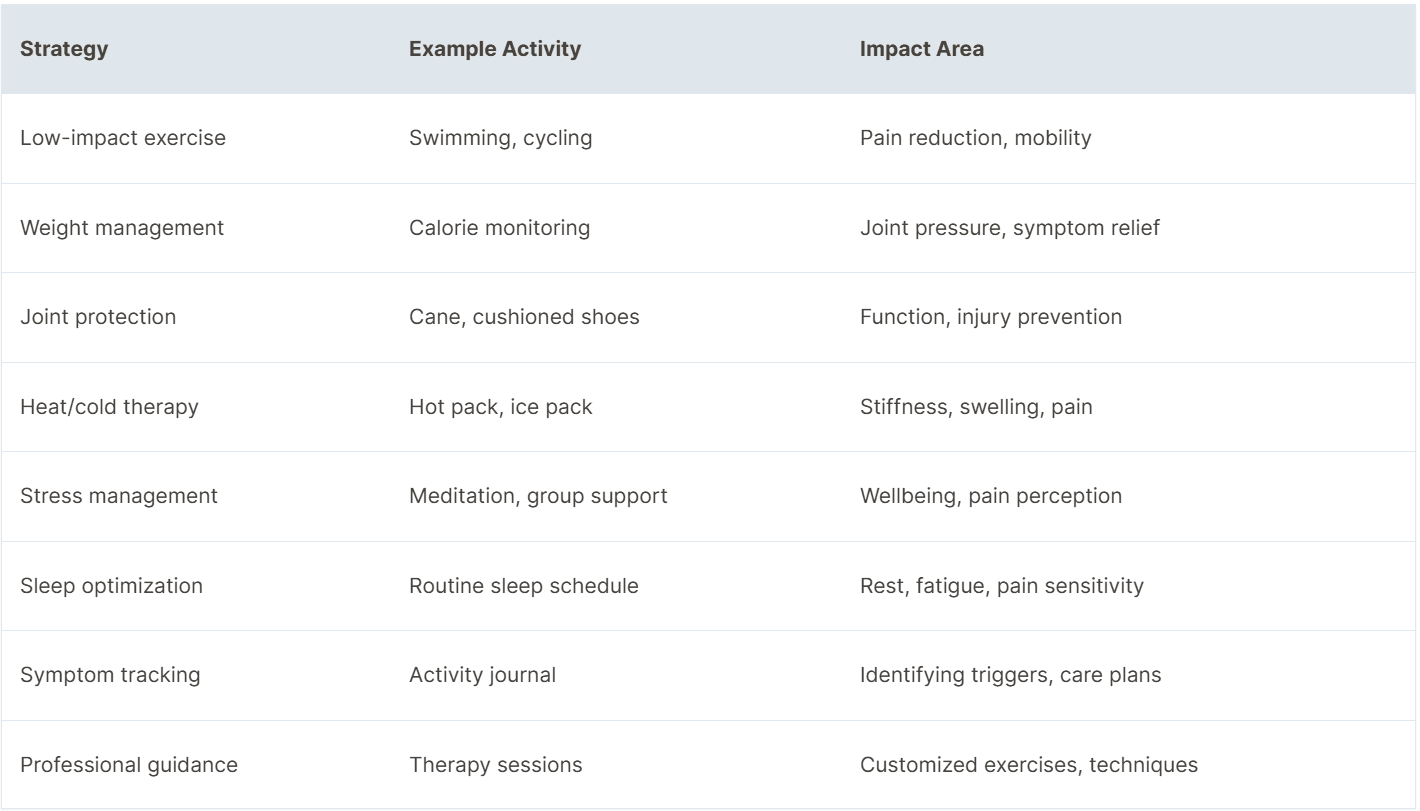
Adopting these strategies for living well with osteoarthritis supports your ability to manage pain and preserve joint function.
Conclusion
Living with osteoarthritis can feel overwhelming but you're not alone on this journey. Small changes in your daily habits and proactive self-care can make a real difference in your comfort and mobility.
Stay curious about new management techniques and keep an open line with your healthcare team. By staying informed and committed to your well-being you'll be better equipped to manage joint pain and maintain your quality of life.


